Nerve Blocks for the Abdomen
Abdominal nerve blocks are a specialized technique in regional anesthesia targeting the nerves in the abdominal wall, providing effective pain relief for various abdominal surgeries. These nerve blocks are highly valued for their ability to significantly reduce the need for systemic opioids, thereby minimizing opioid-related side effects and enhancing postoperative recovery. Nerve blocks are used for a wide range of surgical procedures within the abdomen, from minor outpatient surgeries to major abdominal surgeries, such as hernia repairs, appendectomies, cesarean sections, and laparotomies. Additionally, abdominal nerve blocks have utility in managing acute and chronic pain syndromes, including acute pancreatitis, chronic abdominal pain, and as part of multimodal analgesia in palliative care settings (1).
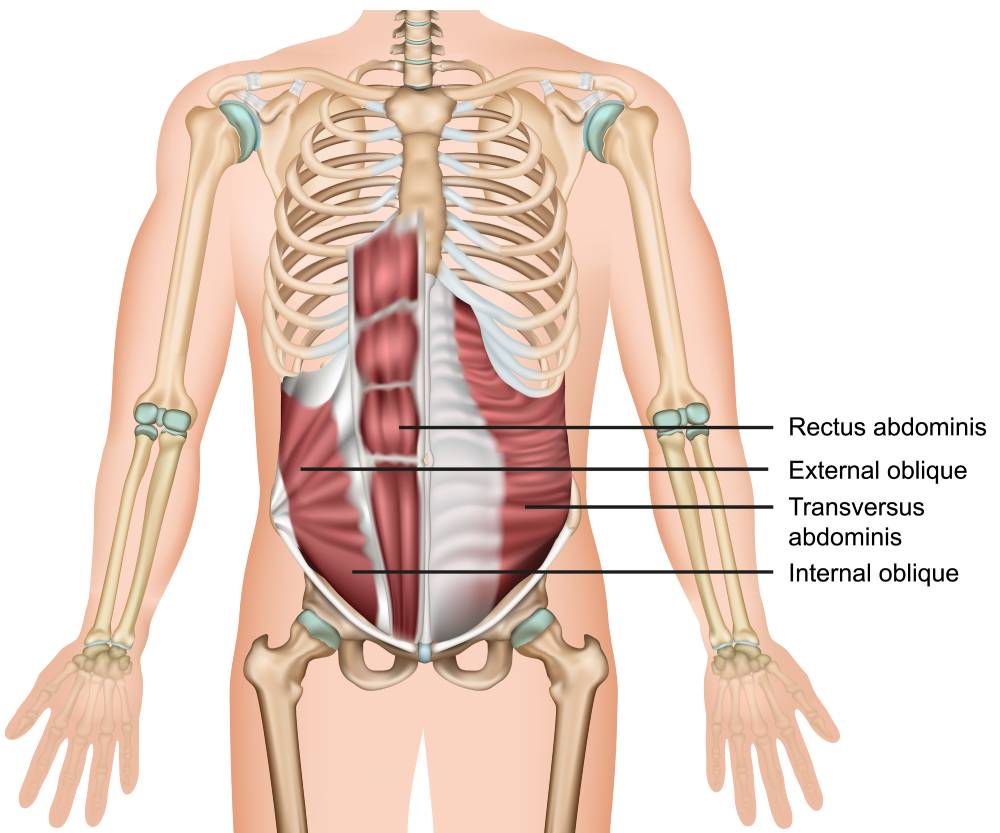
The effectiveness of abdominal nerve blocks depends on a detailed understanding of the abdominal wall’s innervation. The abdominal wall is primarily innervated by the thoracoabdominal nerves (T7-L1), which traverse through the muscle layers of the abdomen. Techniques such as the transversus abdominis plane (TAP) block target these nerves by depositing local anesthetic in the fascial plane between the internal oblique and transversus abdominis muscles (2). This block effectively numbs the anterolateral abdominal wall, making it suitable for surgeries involving these regions. On the other hand, the rectus sheath block is employed to anesthetize the midline by targeting the terminal branches of the thoracoabdominal nerves as they penetrate the posterior aspect of the rectus sheath.
Abdominal nerve blocks are performed in various ways to meet the anatomical and surgical needs of each patient. The lateral transversus abdominis plane (TAP) block is frequently used for surgeries involving the lower abdomen, while the subcostal approach is preferred for procedures affecting the upper abdomen. The posterior approach to the TAP block and the quadratus lumborum block provides more extensive coverage and is beneficial for surgeries with a broader abdominal impact (3).
The advent of ultrasound guidance has revolutionized the techniques used for administering nerve blocks in the abdomen. Ultrasound allows for real-time visualization of anatomical structures of the abdominal wall, the advancing needle, and the distribution of local anesthetic, significantly improving the accuracy and safety of these blocks. This technological advancement has led to the refinement of traditional approaches and the development of new nerve blocks for the abdomen, such as the quadratus lumborum block, which expands analgesic coverage to the lateral and posterior abdominal wall (3).
Despite the many benefits, the use of nerve blocks in the abdomen is not without potential complications. Local anesthetic systemic toxicity (LAST) remains a rare but serious concern, requiring vigilance in adhering to recommended local anesthetic dosages and the use of lipid emulsion therapy as an antidote in the event of toxicity. Other complications may include hematoma, injection site infection, and transient nerve injury. The risk of inadvertent visceral or vascular puncture, although minimal with ultrasound guidance, underscores the need for proficiency in ultrasound techniques and a deep understanding of abdominal anatomy (4).
Abdominal nerve blocks are a dynamic and integral part of modern anesthesia practice. Their use spans a wide range of surgical and pain management scenarios, providing tailored analgesia with a favorable safety profile. Ongoing advances in ultrasound technology and regional anesthesia techniques promise to further improve the efficacy and safety of nerve blocks for the abdomen, solidifying their role in the perioperative management of abdominal surgery.
References
- Chin KJ, McDonnell JG, Carvalho B, Sharkey A, Pawa A, Gadsden J. Essentials of Our Current Understanding: Abdominal Wall Blocks. Reg Anesth Pain Med. 2017;42(2):133-183. doi:10.1097/AAP.0000000000000545
- Tsai HC, Yoshida T, Chuang TY, et al. Transversus Abdominis Plane Block: An Updated Review of Anatomy and Techniques. Biomed Res Int. 2017;2017:8284363. doi:10.1155/2017/8284363
- Liu X, Song T, Chen X, Zhang J, Shan C, Chang L, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative analgesia in patients undergoing abdominal surgeries: a systematic review and meta-analysis. BMC Anesthesiol. 2020;20(1):65. doi:10.1186/s12871-020-00967-2
- Urits I, Ostling PS, Novitch MB, et al. Truncal regional nerve blocks in clinical anesthesia practice. Best Pract Res Clin Anaesthesiol. 2019;33(4):559-571. doi:10.1016/j.bpa.2019.07.013