Cardiac Bypass vs. Stenting
Coronary artery disease (CAD) is the leading cause of morbidity and mortality worldwide, accounting for around 20% of fatalities in the United States.8 CAD is caused by atherosclerosis, which leads to plaque formation in the coronary artery lumen and a reduction in blood flow and oxygen delivery to the heart muscle.8 CAD treatment aims to alleviate angina symptoms and avoid acute myocardial infarction or premature death.6 Revascularization options for individuals with severe coronary artery disease and low ejection fraction include coronary artery bypass graft surgery or percutaneous coronary intervention.4 These two techniques restore adequate blood supply to undersupplied myocardial regions caused by severe coronary stenosis or vascular obstruction.6 A patient’s cardiac care team must decide whether bypass or stenting is most appropriate based on the patient’s condition and risks.
Coronary artery bypass grafting (CABG) is a major surgical procedure in which harvested venous or arterial conduits (donor blood vessels) are used to bypass obstructions in a patient’s coronary arteries.3 The bypass procedure helps to alleviate anginal symptoms by re-establishing blood flow to the heart muscle, which in turn helps to restore function and viability.3 There are two kinds of CABG surgical procedures: on-pump and off-pump.3 During an on-pump CABG, the patient’s heart is arrested, and a cardiopulmonary bypass circuit is used.3 Off-the-pump CABG avoids cardiopulmonary bypass, which reduces perioperative myocardial damage, stroke, neurocognitive impairment, and cardiac-related mortality.9 However, off-the-pump CABG is not appropriate for all patients. The graft type and placement are determined by the patient’s anatomy and the location of the blocked arteries.3 The left internal mammary artery (LIMA) and saphenous vein grafts from the lower extremities are the most routinely employed bypass graft conduits.3 However, the LIMA is the conduit of choice for grafting to the left anterior descending artery, whereas the other conduits are utilized for the other occluded arteries.3
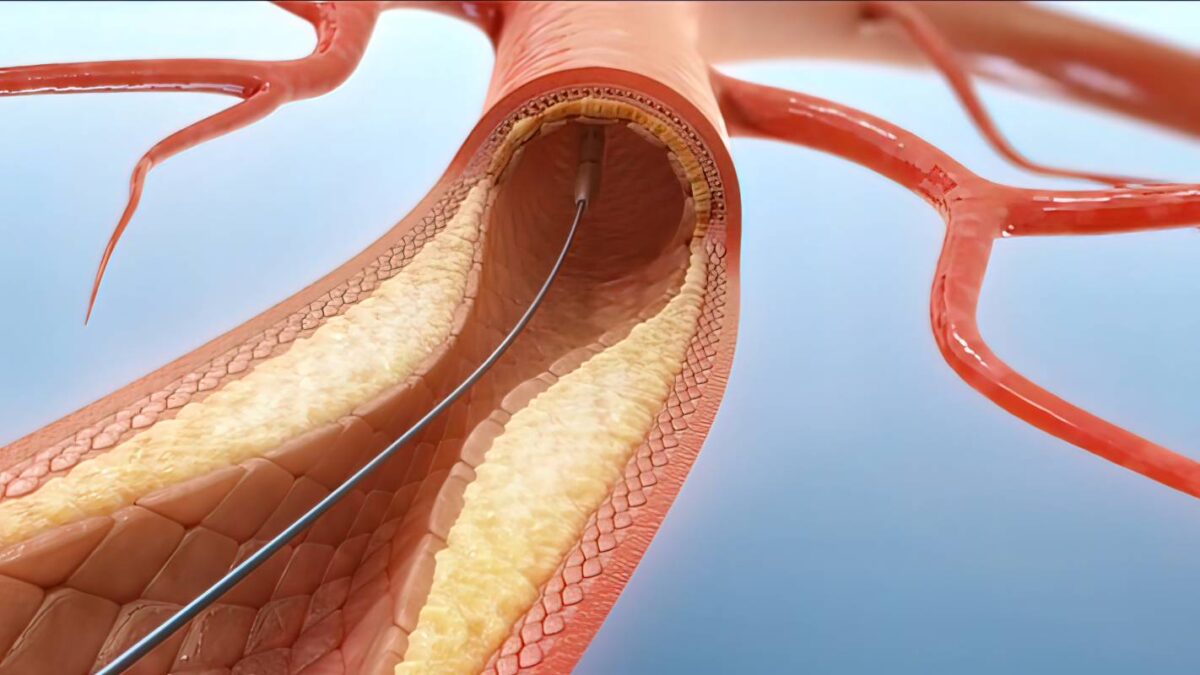
Percutaneous coronary intervention (PCI) is the preferred treatment for unstable angina, myocardial infarction, and spontaneous coronary artery perforation.5 PCI, formerly known as angioplasty with stenting, is a minimally invasive procedure that utilizes a catheter to insert a stent to open clogged or narrow coronary arteries restricted by atherosclerosis-related plaque development,7 and has a number of benefits compared to cardiac bypass surgery. The procedure involves inserting an inflatable balloon-tipped catheter through the skin of the extremities and inflating once it has traversed the target artery site.3 This normalizes the blood flow to the heart muscle by pushing the atherosclerotic intraluminal plaque against the artery wall and widening the available space in the blood vessel for blood to flow.5
Cardiac bypass is generally recommended when there are high-grade blockages in any significant coronary arteries and stenting has failed to clear the blockages.3 CABG has a higher survival rate than PCI in individuals with severe coronary artery disease, multivessel disease, and diabetes.12 As a result, CABG has come to be regarded as the gold standard in the treatment of severe coronary artery disease.2 Although nearly 400,000 CABG operations are performed annually, making it the most frequent major surgical procedure, recent surgical trends have shown a downward trend.3 This downward trend in the use of cardiac bypass is due to the increased use of alternative treatment options, such as medical therapies and stenting, which are more effective in other situations.3 PCI is the treatment of choice for acute myocardial infarction (heart attack).10 Coronary stents increased the safety and effectiveness of percutaneous revascularization.11 Physicians have become increasingly skilled at percutaneous revascularization, often treating patients with CAD that would previously have required CABG. Consequently, the comparative value of CABG and PCI-stenting has been called into question.11
References
- Abdallah MS, Wang K, Magnuson EA, et al. Quality of life after PCI vs CABG among patients with diabetes and multivessel coronary artery disease: a randomized clinical trial. JAMA. 2013;310(15):1581-1590. doi:10.1001/jama.2013.279208
- Ahn, J. M., Park, D. W., Lee, C. W., Chang, M., Cavalcante, R., Sotomi, Y., Onuma, Y., Tenekecioglu, E., Han, M., Lee, P. H., Kang, S. J., Lee, S. W., Kim, Y. H., Park, S. W., Serruys, P. W., & Park, S. J. (2017). Comparison of Stenting Versus Bypass Surgery According to the Completeness of Revascularization in Severe Coronary Artery Disease: Patient-Level Pooled Analysis of the SYNTAX, PRECOMBAT, and BEST Trials. JACC. Cardiovascular interventions, 10(14), 1415–1424. https://doi.org/10.1016/j.jcin.2017.04.037
- Bachar, B. J., & Manna , B. (2022). Coronary Artery Bypass Graft. In StatPearls. StatPearls Publishing.
- Chen, Y. W., Lee, W. C., Fang, H. Y., Sun, C. K., & Sheu, J. J. (2022). Coronary Artery Bypass Graft Surgery Brings Better Benefits to Heart Failure Hospitalization for Patients with Severe Coronary Artery Disease and Reduced Ejection Fraction. Diagnostics (Basel, Switzerland), 12(9), 2233. https://doi.org/10.3390/diagnostics12092233
- Chhabra, L., Zain, M. A., & Siddiqui, W. J. (2022). Angioplasty. In StatPearls. StatPearls Publishing.
- Doenst, T., Haverich, A., Serruys, P., Bonow, R. O., Kappetein, P., Falk, V., Velazquez, E., Diegeler, A., & Sigusch, H. (2019). PCI and CABG for Treating Stable Coronary Artery Disease: JACC Review Topic of the Week. Journal of the American College of Cardiology, 73(8), 964–976. https://doi.org/10.1016/j.jacc.2018.11.053
- Percutaneous Coronary Intervention (PCI). (2011, November 6). Cleveland Clinic. Retrieved October 6, 2022, from https://my.clevelandclinic.org/health/treatments/22066-percutaneous-coronary-intervention
- Senst, B., Kumar, A., & Diaz, R. R. (2022). Cardiac Surgery. In StatPearls. StatPearls Publishing.
- Shaefi, S., Mittel, A., Loberman, D., & Ramakrishna, H. (2019). Off-Pump Versus On-Pump Coronary Artery Bypass Grafting-A Systematic Review and Analysis of Clinical Outcomes. Journal of cardiothoracic and vascular anesthesia, 33(1), 232–244. https://doi.org/10.1053/j.jvca.2018.04.012
- Shahjehan, R. D., & Bhutta, B. S. (2022). Coronary Artery Disease. In StatPearls. StatPearls Publishing.
- Thomas P. Wharton, Lorelei L. Grines, Mark A. Turco, James D. Johnston, Jane Souther, David C. Lew, Ajazuddin Z. Shaikh, William Bilnoski, Sushil K. Singhi, A.Ersin Atay, Nancy Sinclair, Dawn E. Shaddinger, Mark Barsamian, Mariann Graham, Judith Boura, Cindy L. Grines, Primary Angioplasty in Acute Myocardial Infarction at Hospitals With No Surgery On-Site (the PAMI-No SOS study) versus transfer to surgical centers for primary angioplasty, Journal of the American College of Cardiology, Volume 43, Issue 11, 2004, Pages 1943-1950, ISSN 0735-1097, https://doi.org/10.1016/j.jacc.2004.03.013.
- Villareal, R. P., Lee, V. V., Elayda, M. A., & Wilson, J. M. (2002). Coronary artery bypass surgery versus coronary stenting: risk-adjusted survival rates in 5,619 patients. Texas Heart Institute journal, 29(1), 3–9.