The Influence of Neostigmine on Early Postoperative Cognitive Dysfunction
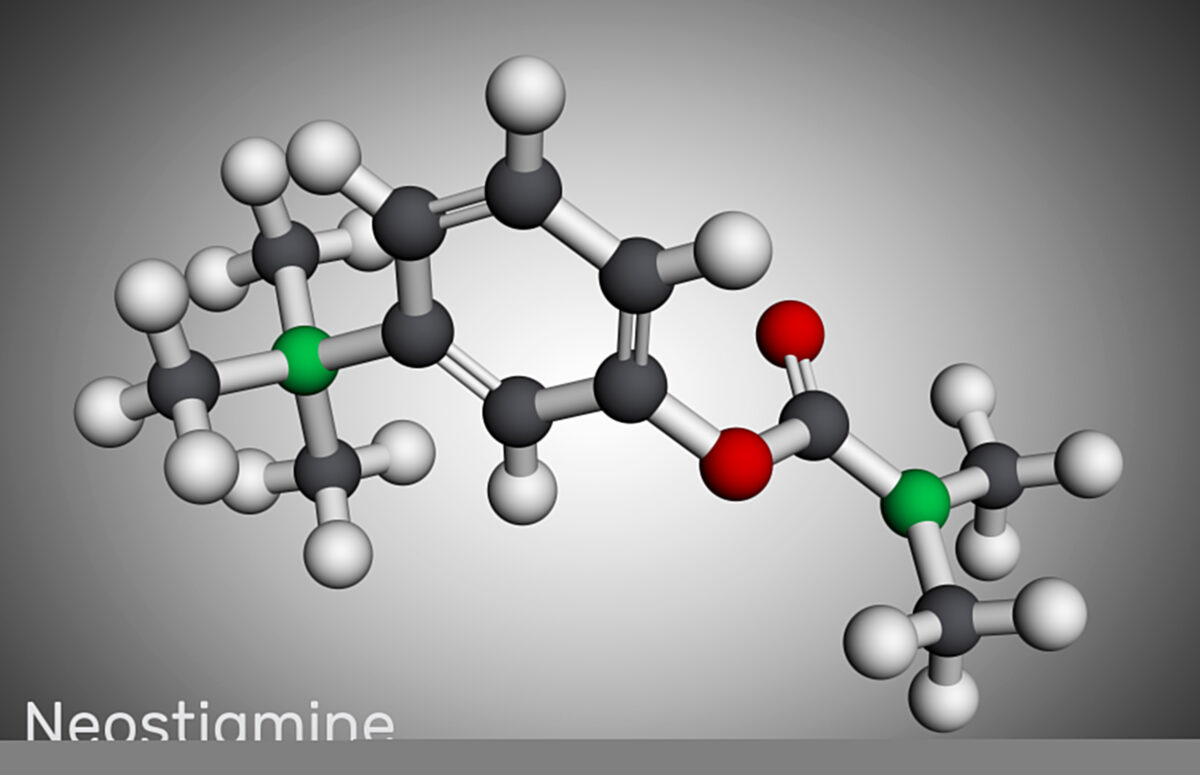
Neostigmine, a well-known anticholinesterase medication, has been extensively used in the medical field, particularly in the management of myasthenia gravis and as an antidote for anticholinergic poisoning. However, its influence on cognitive functions, especially in the context of early postoperative cognitive dysfunction (POCD), has become a subject of increasing interest among researchers and clinicians.
Early POCD is a common complication following surgery, particularly in elderly patients, and is characterized by a temporary but significant decline in cognitive abilities such as memory, concentration, and processing speed. The etiology of POCD is multifactorial, involving factors such as patient age, type of anesthesia, surgical stress, and the use of certain medications during the perioperative period. The impact of neostigmine on cognitive functions post-surgery is a complex interplay of various mechanisms.
Neostigmine, by inhibiting acetylcholinesterase, increases the level of acetylcholine in the synaptic cleft. Acetylcholine is a critical neurotransmitter involved in learning, memory, and other cognitive processes. In theory, increasing acetylcholine availability should enhance cognitive function. However, the reality is more nuanced. Several studies have indicated that the administration of neostigmine, particularly at higher doses, may be associated with an increased risk of POCD. This adverse effect could be attributed to the excessive cholinergic activity leading to a phenomenon known as ‘cholinergic overdrive’, which paradoxically may impair cognitive functions.
Moreover, neostigmine’s influence on cerebral blood flow and oxygenation is another aspect to consider. While adequate cerebral perfusion is essential for optimal cognitive function, alterations in cerebral hemodynamics caused by neostigmine might contribute to cognitive impairment in the vulnerable postoperative period. For instance, neostigmine-induced bradycardia can lead to decreased cardiac output, potentially reducing cerebral perfusion and oxygenation, thus affecting cognitive abilities.
Another significant aspect is the interaction of neostigmine with other medications commonly used in the perioperative period, such as anesthetics and analgesics. These interactions can have synergistic, additive, or antagonistic effects on cognitive functions. For instance, the interaction of neostigmine with certain anesthetics might exacerbate the cognitive dysfunction seen in early POCD.
Furthermore, patient-specific factors such as age, pre-existing cognitive impairment, and genetic predispositions play a crucial role in determining the impact of neostigmine on cognitive functions postoperatively. Elderly patients, who are already at a higher risk for POCD, might be more susceptible to the cognitive effects of neostigmine. Genetic variations in enzymes metabolizing neostigmine could also influence its effects on cognition.
The duration of action and timing of administration of neostigmine in relation to surgery are other critical factors. The timing of administration could influence the peak concentration of the drug during critical periods of cognitive processing. Additionally, prolonged exposure to neostigmine, especially in cases of repeated dosing, might have a cumulative effect on cognitive functions.
Current research into the effects of neostigmine on early POCD is ongoing, with studies employing various methodologies, including randomized controlled trials, observational studies, and cognitive assessments. These studies aim to delineate the precise mechanisms by which neostigmine influences cognitive functions and to identify the patient populations most at risk.
In conclusion, the influence of neostigmine on early postoperative cognitive dysfunction is a multifaceted issue. While the theoretical basis suggests potential cognitive benefits due to increased acetylcholine levels, clinical observations and research indicate a more complex relationship, potentially involving cholinergic overdrive, altered cerebral hemodynamics, drug interactions, and patient-specific factors. Understanding this relationship is crucial for optimizing perioperative care, especially in vulnerable populations such as the elderly, and for developing strategies to mitigate the risk of POCD. Future research in this area is essential to gain a more comprehensive understanding and to guide clinical practice.